Free Standard Shipping on All Orders $285


The OsteoGen® Bone Grafting Plug is an easy and affordable way to clinically deliver bone graft. It’s mainly used for ridge maintenance and socket preservation.

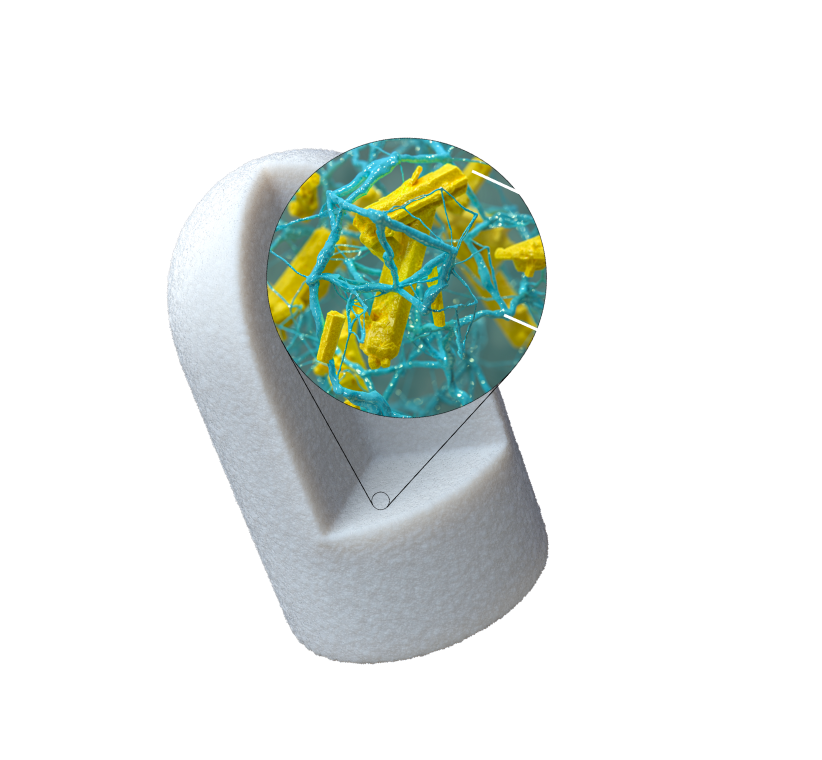
The idea is simple: a collagen plug is filled with OsteoGen® non-ceramic bone graft crystals. This creates the OsteoGen® Bone Grafting Plug.

The result is a bone graft combined with a collagen plug for ease of clinical delivery—without the need for a membrane.

The OsteoGen® Bone Grafting Plug combines Bioactive Resorbable Calcium Apatite with a bovine Achilles tendon collagen matrix. This creates a structure that mimics the organic and inorganic components of physiologic bone.

OsteoGen® is a bioactive and resorbable calcium apatite-based bone graft. It is physiochemically and crystallographically similar to human bone.1

The OsteoGen® non-ceramic production process yields a resorbable bone graft with a unique Ca:P ratio. It is NOT a -TCP and NOT a non-resorbable dense ceramic HA (nor is it a biphasic mixture of the two).

The Bovine Achilles Tendon collagen carries the bone graft for easy and efficient delivery to the site. Thus, the hassle and time spent mixing and packing particulate bone grafts is eliminated—and so is the potential for particulate wash out.

The Type I collagen acts as a wound dressing—not only to stabilize the clot, but also to absorb and deliver blood flow to the slowly resorbing graft (a feature critical for the initiation of bone formation and early angiogenesis).

The collagen found in the OsteoGen® Plug provides a scaffold for keratinized tissue to develop over the grafted site.

The OsteoGen® Bone Grafting Plug will show radiolucent on the day of placement. It becomes radiopaque in 3–5 months when it has been replaced with host bone. Implant placement can then be achieved.





Clinical images courtesy of Brigham Stoker DDS
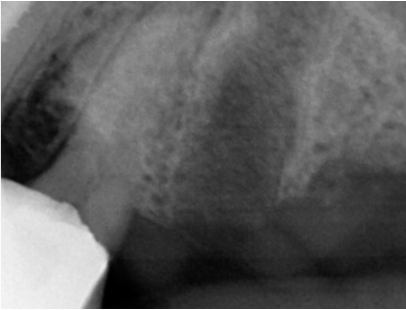
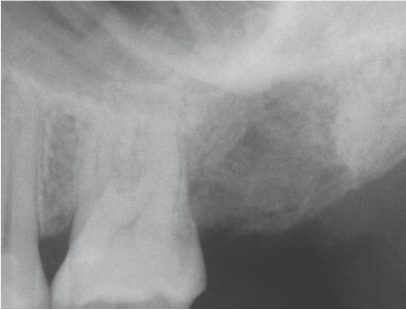
Pre-operative x-ray of Tooth #12 to be extracted. Tooth #13 was extracted
two months prior and was grafted with an OsteoGen® Plug.

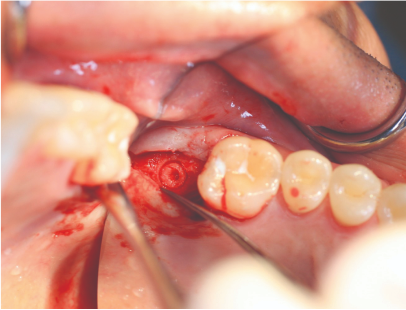
Extraction of Tooth #12.

The surgical site was initially debrided to induce bleeding and establish the Regional Acceleratory Phenomenon.

Appropriately sized OsteoGen® Plugs were inserted, and blood was allowed to absorb.
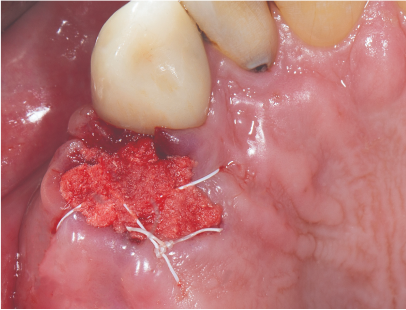
After insertion of OsteoGen® Plugs, the socket was sutured over top. No membrane was requried.
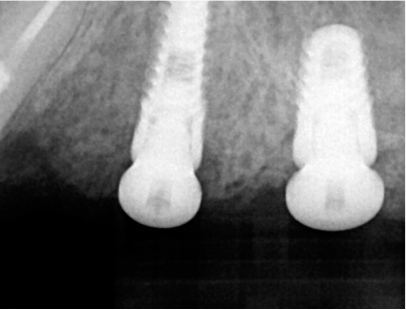
Two implants placed four months later—with a sinus bump on the distal implant.
Clinical images courtesy of German Murias DDS, ABOI/ID
OsteoGen® is a low density bone graft and the OsteoGen® Plugs will show radiolucent on the day of placement.
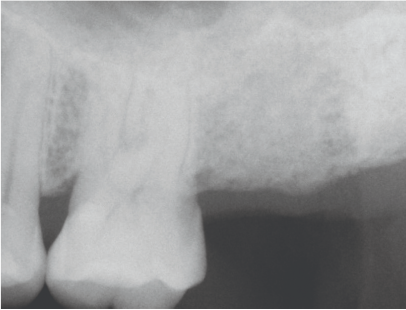
As the OsteoGen® crystals are resorbed and replaced by host bone, the site will become radiopaque.

The collagen promotes keratinized soft tissue coverage over the graft.
Solid bone is seen upon reentry prior to implant placement. In this image, a core sample was retrieved.
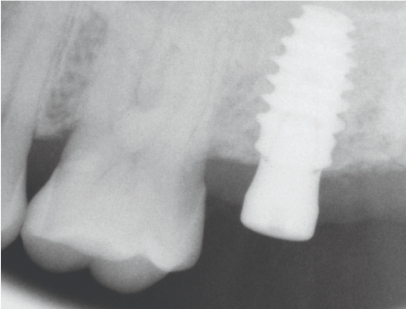
Implant is placed. Note the histology below showing mature osteocytes in lamellar bone formation.
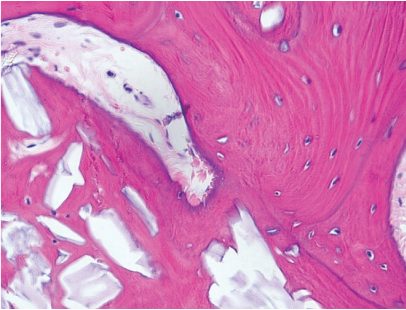
Some of the larger OsteoGen® crystals and clusters are slowly resorbing. Bioactivity is demonstrated by the high bone to crystal contact absent of any fibrous tissue encapsulation.3-4
1. Valen M, Ganz SD. A synthetic bioactive resorbable graft for predictable implant reconstruction: part one. J Oral Implantol. 2002;28(4):167-77. 2. Frost HM. The regional acceleratory phenomenon: a review. Henry Ford Hosp Med J. 1983;31(1):3-9. 3. Spivak JM, Ricci JL, Blumenthal NC, Alexander H. A new canine model to evaluate the biological response of intramedullary bone to implant materials and surfaces. J Biomed Mater Res. 1990;24(9):1121-1149. doi:10.1002/jbm.820240902. 4. Ricci JL, Blumenthal NC, Spivak JM, Alexander H. Evaluation of a lowtemperature calcium phosphate particulate implant material: physical-chemical properties and in vivo bone response. J Oral Maxillofac Surg. 1992;50(9):969-978.
or Shop Now »
